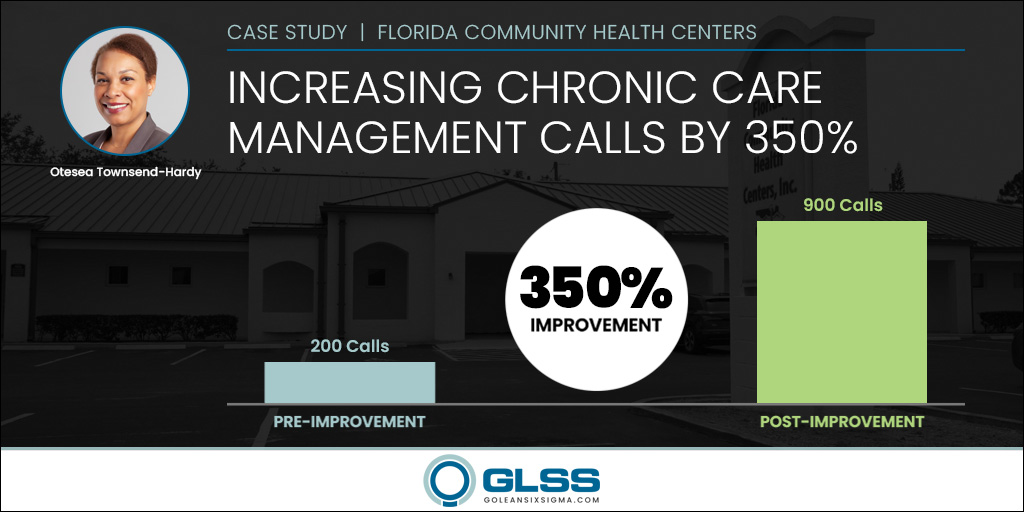
Increasing Chronic Care Management Calls by 350% at Florida Community Health Centers (FCHC)
Home » Case Study » Increasing Chronic Care Management Calls by 350% at Florida Community Health Centers (FCHC)
Florida
Healthcare
Patient Care
350%
PROJECT SUMMARY
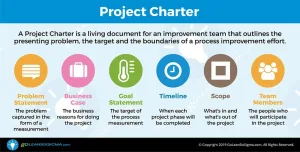
- Business Case: In the last 3 months, the Chronic Care Management (CCM) 20-minute calls have declined to 206 per month. If the problem persists we reduce the continuity of care as a patent-centered medical provider. Improving the number of calls and patients supported results in an enhanced clinical experience and fosters care coordination activities. Improved services could also translate to increased revenue, as more calls add additional reimbursement.
- Root Cause Analysis:
- Staff not knowledgeable of EMR system capabilities
- Staff unaware of latest requirements
- Number of manual steps
- Solutions Implemented:
- Distribute educational materials
- Validate reporting
- Utilize System Care Plan Module
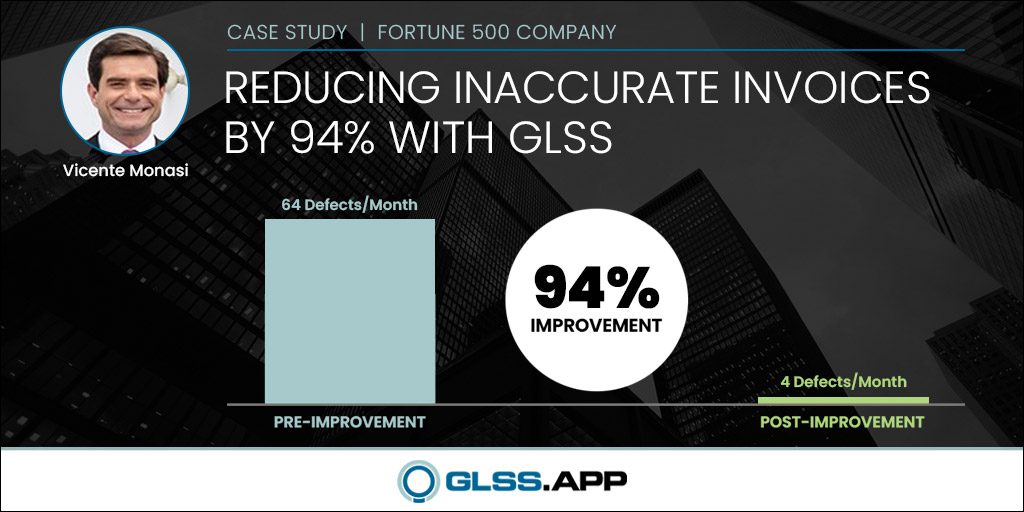
- Project Result: Increased calls from 200 to over 1,000 consistently per month. Increased revenue an average of $30,000 per month.
In recent months, the number of Chronic Care Management (CCM) 20-minute telephone calls has declined to 200 per month, representing only 17% of the chronically ill patient population that Florida Community Health Centers (FCHC) serves.
In 2015, the Centers for Medicare & Medicaid Services (CMS) initiated the Chronic Care Management (CCM) program to decrease healthcare spending by focusing on the needs of patients with two or more chronic conditions. This program reimburses medical practitioners for contacting patients once a month for at least 20 minutes to meet the patient’s ongoing needs.
Since 1976, FCHC has been a healthcare leader in Florida. They provide comprehensive primary and specialty healthcare and patient support services through a network of centers surrounding Lake Okeechobee and across Florida’s Treasure Coast. Their mission is to ensure everyone in their communities has access to culturally competent, high-quality, affordable healthcare.

Project Team: Kerri Daniels, MD; Jeremiah Barham; Oteasa Townsend-Hardy; Christine Colby; Alejandro Miquel, MD
FCHC has created a “one-stop shop” for patients and provides an extensive range of Pediatric and Adult care. They are recognized as a Patient-Centered Medical Home (PCMH) by the National Committee for Quality Assurance (NCQA).
Patients with complex conditions usually see more than one physician and undergo multiple lab tests and procedures. When those patients have a medical home, care can be better coordinated by their primary care physician. The medical home model provides a central point to make decisions and provide care. CCM calls are a critical component of the medical home model.
Otesea Townsend-Hardy is the Senior Director of Quality Improvement (QI), Compliance, and Communications at FCHC. She has extensive experience working with care providers, managed care, and payers. This expertise along with her nursing and QI background, uniquely qualifies her to lead FCHC improvement efforts. Otesea says, “Our patients benefit from a ‘medical home’ model, where they may access our extensive array of healthcare clinicians and services in an atmosphere where they are treated with respect, care, and concern.
As a patient-centered medical home, our mission is to ensure care coordination. With our current CCM call level, we reduce the continuity of care and negatively impact patient outcomes for a chronically ill population. We are not fulfilling our mission and we could lose revenue, further impacting our ability to fulfill our mission.”
Otesea says, “We are a Federally Qualified Health Center (FQHC) and we strive to meet the needs of an underserved area or population. The ultimate goal is to improve outcomes but also gain revenue. I did a baseline of the CCM calls and I coached the team that if we can improve our CCM call volume, we can change lives. That triggered a deeper dive into the chronic care management calls and the patient population that needs it.”
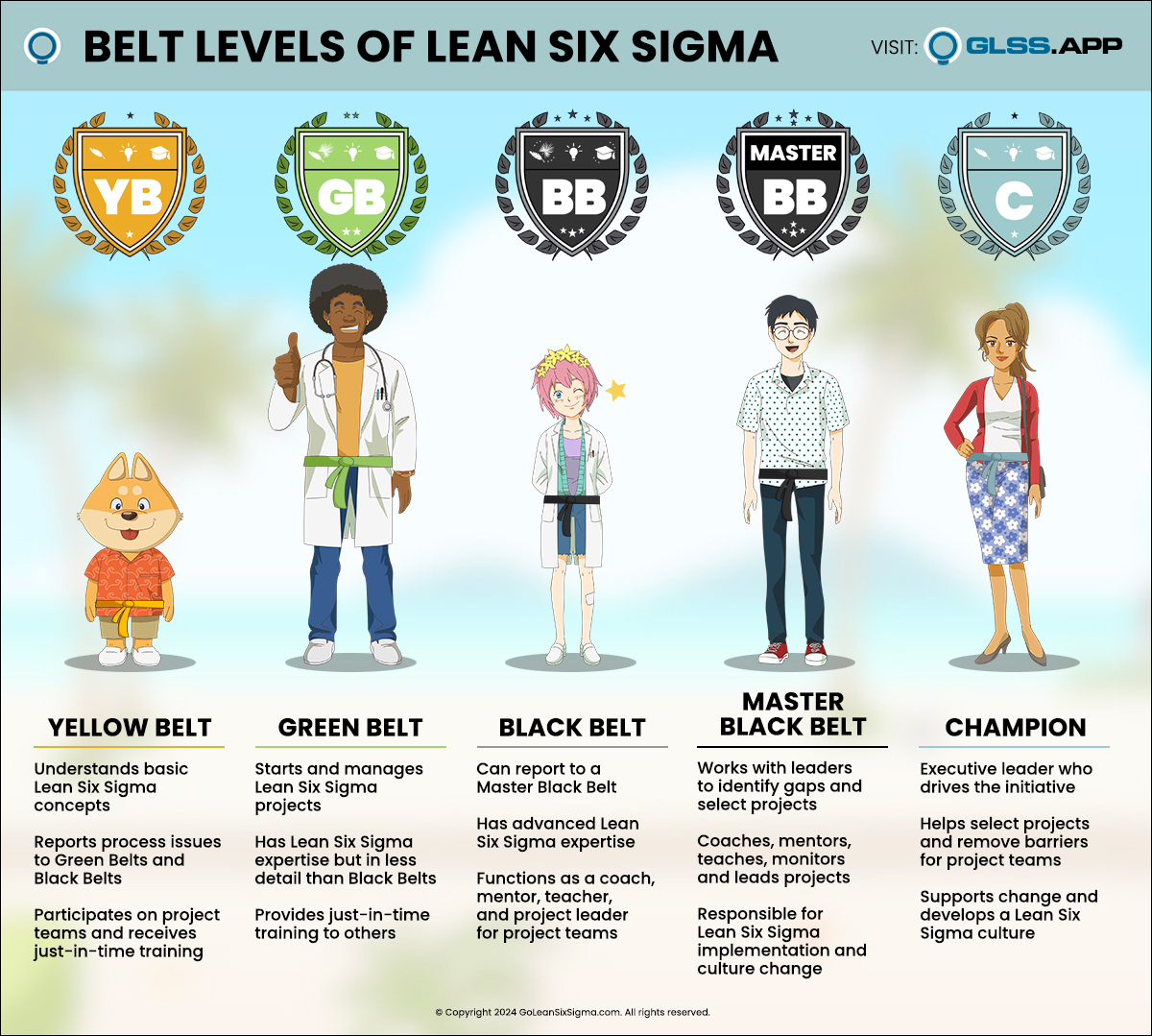
Otesea’s unique background helps her see the big picture. She says, “Having dealt with hospitalization and utilization reviews, coordinating care plans combined with my background in QI and nursing, I saw an opportunity to make a real impact. I decided to take the GLSS Lean Six Sigma Black Belt Training & Certification to hone my QI skills and better pursue this opportunity.”
“I saw an opportunity to make a real impact. I decided to take the GLSS Lean Six Sigma Black Belt Training & Certification to hone my [Quality Improvement] skills.”
When the team dug into the CCM call process, it became immediately clear there was a mountain of opportunities to address.
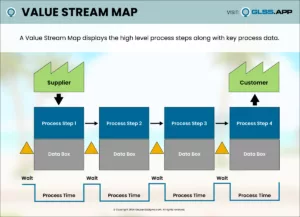
Otesesa says, “Process Mapping and the Process Walk were the most useful tools for this project. They helped us understand what was happening now. Later, they helped us create the new process.
Our process was not clearly defined. As we continued our investigation, there were a few surprises. CMS requires you to document and calculate at least 20 minutes of patient call time to be able to bill for the service. We were performing tasks that should be documented. For example, staff didn’t realize that email communications counted towards the 20 minutes of call time. For the CCM calls, knowing the process requirements is essential.”

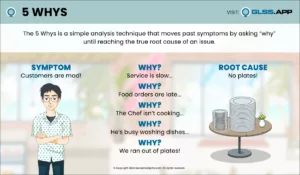
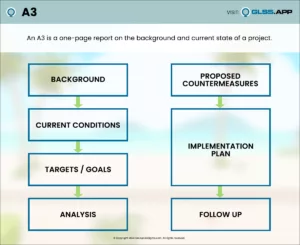
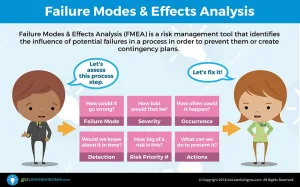
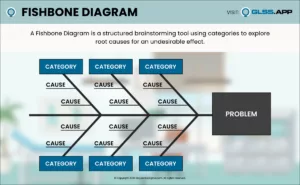
Using the insights gained from the Process Walk, the team performed a Root Cause Analysis using the Fishbone Diagram and 5 Whys learned in the GLSS training. The critical findings and root causes discovered included:
- Several activities of call time that were performed were consistently missing CMS required documentation
- Time wasted searching in the electronic medical record (EMR) for care plan notes because of disorganization
- Excessive time and variation in the creation of patient care notes
- Care Managers or Care Coordinators do not always complete the care plan
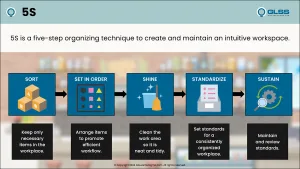
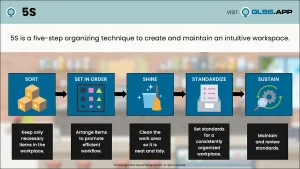
Walking the process made it clear the team needed to create Standard Work—a detailed definition of the current best practices for performing a process. The team created the easiest, most waste-free, and effective way to perform the work by:
- Educating everyone on the CMS and process requirements
- Clarifying roles and responsibilities
- Removing waste and inefficiencies
- Reallocating staff to ensure key tasks were adequately covered
- Cross-training staff to use an existing tool within the EMR that enables care providers to easily build personalized care plans, enter real-time updates, and manage care plan meetings
- Identifying activities for calls in a central area within the EMR
- Refining care plan guidelines to be user-friendly and consistent
After implementing the new process, the staff was able to increase the calls from 200 a month to 900 a month— a 350% improvement. The Medicare population in the FCHC service area is around 1,100 patients. Nine hundred calls a month is more than an 80% patient participation rate.

Also, the team saved time working in the EMR, allowing Care Managers to outreach to additional patients when volume requires more staff.
Otesea says, “Because we can make these calls, you have licensed nurses making sure that patients are getting the care they need. For example, on a recent call, the nurse noticed the patient hadn’t picked up their blood pressure medication. The nurse had our in-house pharmacy mail it to them. Now, the patient is taking their medication and they didn’t need to get in a car and drive to the pharmacy. The benefit to the patient is a better quality of care. The benefit to FCHC is serving this population in need and generating an additional $30,000 per month in revenue, enabling us to continue our mission to serve the underserved. It’s a win/win!
Thanks to our improved ability to reach out to patients, many more are receiving the care they need.”